Uhc Vision Plan Out Of Network Claim Form – An ERISA Portion 502(a) program might be claimed in a number of methods. Both for dental and medical solutions, boasts types can be found. Your medical provider will need you to total and distribute these claim paperwork to UnitedHealthcare. To save you time, assert kinds can easily be bought inside the workplaces of countless contributing companies. Soon after accomplishing the shape, you might send out it right to UnitedHealthcare. Visit your health insurance representative or contact UnitedHealthcare if you need help filling out your form.
Assert Form for ERISA Area 502(a) Strategies
A particular period of time have to complete well before publishing an ERISA Portion 502(a) program claim form. In this particular period of time, a fiduciary task state or reward denial assert needs to be manufactured. Federal and state regulations manage ERISA portion 502(a) claims.
The EBSA will levy a civil fine on you if you don’t adhere to this timeline. The civil okay is determined as being a percentage in the plan’s disgorged losses and profits. The fiduciaries, who are accountable for make payment on good, might be held accountable for it.
If you have a plan that does, review the claim form to make sure it complies with ERISA regulations. A venue exclusion supply may be incorporated into a plan. Within your SPD and also in your communications with members, be sure to mention the venue restriction. However, you should refrain from saying anything unnecessarily since it can be used against you in court. In almost any celebration, ensure that you consult with the legitimate advise for your want to promise conformity.
Five percent of the amount at issue is the penalty sum. You may, however, ask for a penalty waiver if you miss the payment deadline. If a fine is excessively high, it is not waived. If you can pay it, you should pay the penalty. It must be paid for within two months. If you miss the deadline, the EBSA will issue a revised penalty notice.
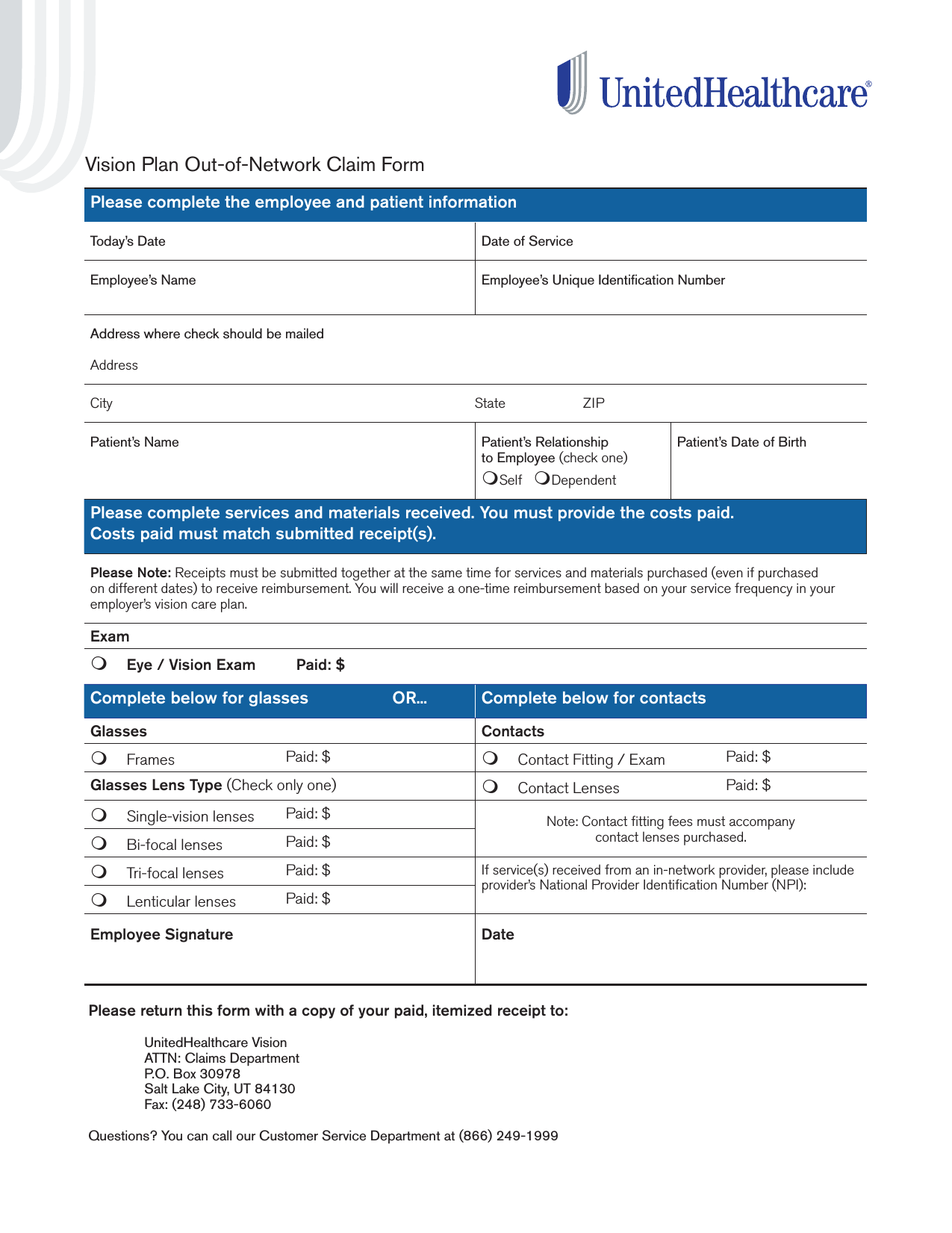
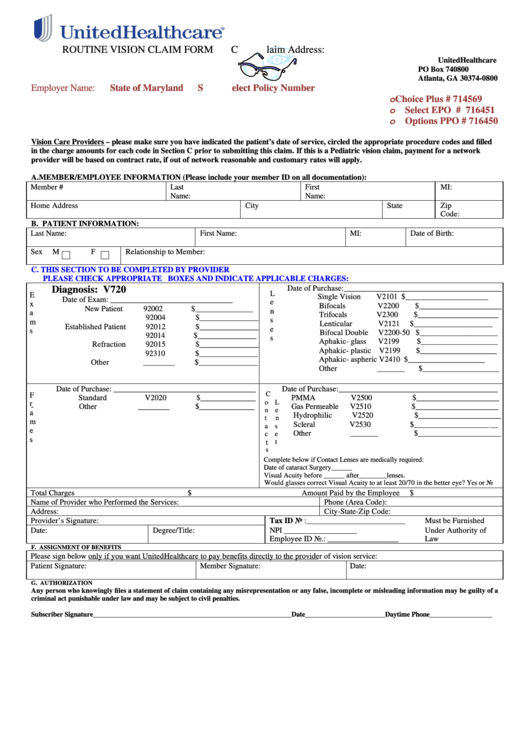
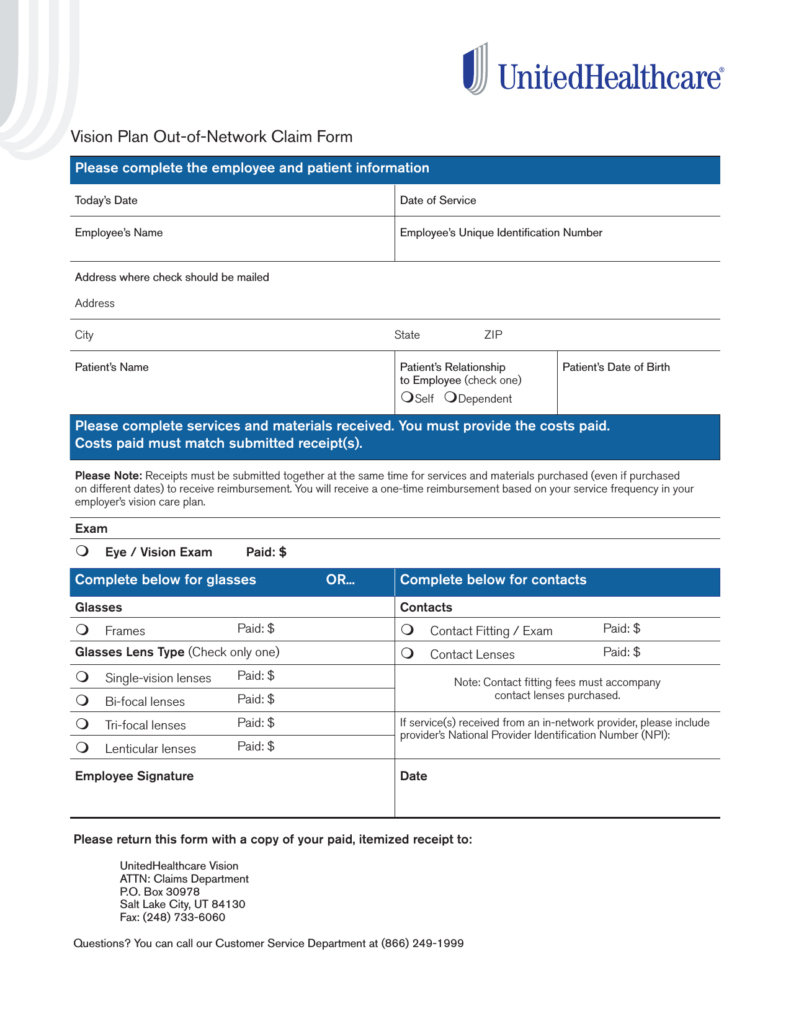
Kind for medical care claims
You must involve all required specifics when sending a health-related professional services declare. As an illustration, you will need to range from the service’s time as well as place. If you are filing a claim from outside the country, you must also attach documentation of travel. You can ask for assistance from your wellbeing treatment provider’s invoicing division. In order to record all medical costs, section D must also be completed.
UnitedHealthcare will give you the claim form for the medical doctor. It needs to be recently and accurately filled in. To take the settlement, the distributor should have a present Income tax Identification Number. The shape is also accessible in the provider’s business office. To ensure that the insurance company to directly pay the company, you have to make certain that these people have a existing Taxation Detection Number.
Lots of the containers for this kind can also be located on the CMS-1500 develop. It must include information on the sufferer, the specialist, the course of treatment method, as well as any other appropriate info. In order to minimize errors and increase your chances of getting paid, it’s crucial to adhere to the insurance provider’s guidelines. If you provide more details, it is preferable. If the patient was engaged in a car accident, for instance, you should note on the form.
Fill out a CMS-1500 if you need to file a claim for medical services. In order for it to be acknowledged, it should have all important specifics in regards to the wounded party. A copy of the finished develop has to be presented to the sufferer, the patient’s authorized broker, the worker’s settlement insurance company, the employer or self-insured company, and the boss. The Workers’ Settlement Board develop is currently replaced with the CMS-1500.
state develop to get a oral strategy
If the entire fee is not covered by insurance in New York, the dentist may report it on a Dental Plan Claim Form. Except when the individual gets a low cost in the insurance company, the dental practitioner will cost the sufferer the total fee up front. If the patient has a secondary insurance plan and no dental insurance, the dentist can only report the fee that is not covered by the insurance plan.
A claim develop for any dental program contains about three factors. The initial one is to the policyholder and possesses theaddress and name, and birthdate in the protected participant. Before approving a claim, the dental plan must answer the questions in the second part. The patient’s job and academic background, and also other information that could assist the insurance company in finalizing the state, are detailed within the third aspect.